In Vitro Fertilization, or IVF, is a common method of assisted reproduction technology (ART). It’s used to help couples or individuals get pregnant. There are many reasons why someone may choose to pursue IVF. Heterosexual couples who struggle with infertility, single men who wish to have a biological child, and LGBTQ couples often turn to IVF to help them have a baby.
The Basics of In Vitro Fertilization
The IVF process includes a series of medications and medical procedures to create an embryo in a laboratory setting. You will work closely with your fertility clinic to plan your specific course of treatment. It’s used when an individual or a couple are unable to conceive naturally. Rather than sperm fertilizing an egg inside a woman’s body, egg and sperm are extracted from the intended parents and/or donors and combined in the lab. If fertilization is successful and an embryo develops, a doctor will insert the egg into the woman’s uterus so it can implant and develop into a fetus.
Understanding IVF can feel a little intimidating at first. At Family Inceptions, we’ve been immersed in all things reproductive technology for many years, so we’d love to walk you through all the ins and outs of IVF. Let’s explore the details.
What is In Vitro Fertilization (IVF) Treatment?
The Mayo Clinic defines in vitro fertilization as “a complex series of procedures used to help with fertility or prevent genetic problems and assist with the conception of a child.”
“In vitro” is Latin for “in the glass,” and it’s used to describe a medical experiment, study, or procedure outside a living organism. “In the glass” is a fitting term because the procedure takes place in a test tube or Petri dish. You may have heard the term “test tube babies,” which is a term used by the media and laypeople when talking about babies born via IVF.
The first baby to be conceived with IVF was born in 1978 and has since become a very common means to have a child. Science Daily estimates that over 8 million babies have been born as a result of IVF since then.
As you begin more in-depth research into the IVF process, you’ll start to notice a lot of acronyms. The TTC community (trying to conceive) is quite notorious for using shorthand to discuss and describe the path to fertility. We put together a quick guide to help you make sense of it all: Fertility Acronyms Guide.
IVF Success Rate
There are many factors that affect the success rate of IVF. Your age or the age of your egg donor, previous pregnancy and birth history, your BMI, the cause of your infertility (if known and applicable), and the particular fertility clinic you choose can all affect your chances for a successful pregnancy.
According to a study published in 2015, there is a 29.5% chance of having a live birth as a result of the first round of IVF. By the 6th round, approximately two-thirds of all patients had achieved a successful pregnancy that resulted in a live birth. Of course, six rounds is quite a lot, so not all couples get there. IVF is expensive and can be emotionally draining, but your odds do improve with multiple attempts.
The Society for Assisted Reproductive Technology has developed an evidence-based calculator that helps you predict your chance of a successful IVF process. The SART Patient Predictor is free and easy to use.
The Safety and The Risks
IVF is a safe process with few side effects and a low level of risk. Serious complications are rare, but as with any medical procedure, there are some potential problems to be aware of.
The most common side effects occur as a result of taking fertility medications. In order to stimulate egg production, the intended mother or egg donor will take injectable fertility medications. These can cause bloating, cramps, tender breasts, irritation or redness at the injection site, nausea and vomiting, mood swings, and/or fatigue.
There is approximately a 10% chance of developing ovarian hyperstimulation syndrome, or OHSS. Symptoms are usually mild and similar to those listed above, but there is a risk for complications. In severe cases, fluid builds up in the abdomen and lungs. If left untreated, it can result in dehydration, difficulty breathing, severe pain, and rarely, blood clots or kidney failure. The vast majority of OHSS cases resolve after just a few days, but it’s important to pay attention to anything that feels out of the ordinary when undergoing IVF treatments.
There are a few possible risks during the egg retrieval and embryo transfer procedures. Both involve the insertion of a needle or tube into your uterus. As with any invasive procedure, there is a slight risk of infection. The most common side effect is abdominal pain/cramping, but this can almost always be controlled with over-the-counter pain medication. More severe side effects are very rare but can include injury to internal organs near the uterus or pelvic infection. Following the embryo transfer, many women report light bleeding and mild cramping.
Some sources note that babies born via IVF have a small risk of having birth defects. About 4% of babies born via IVF develop birth defects, but the numbers are very close to what occurs in the general population.
The biggest risk to both the fetus and the mother or gestational carrier is the chance for multiple pregnancy. Twin, triplet, or multiple pregnancies are at higher risk for miscarriage, birth defects, anemia, gestational hypertension, and premature birth. As many as 60% of all twins and almost all higher numbers of multiples are born premature, before 37 weeks gestation. This means lower birth weight and possible immature lungs or other organs.
Discuss the risk of multiples with your IVF doctor. Many clinics will only implant one embryo specifically to avoid a multiple pregnancy. If you choose to implant more than one embryo to increase the chance of a successful pregnancy, you will need to consider the risk involved in more than one embryo begins to develop.
The Process of In Vitro Fertilization Treatment
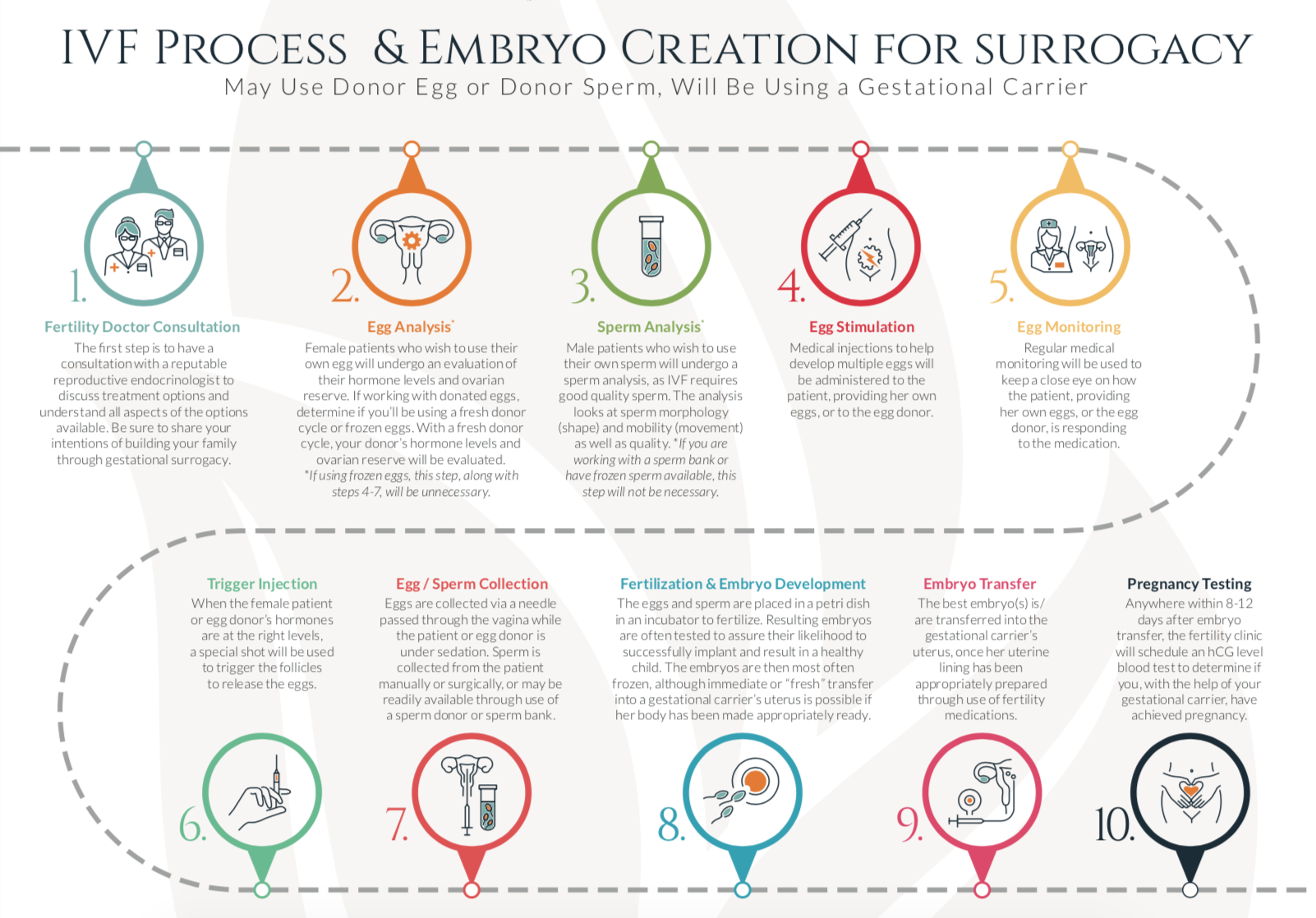
The IVF process involves many steps, from preparing your body and menstrual cycle to egg retrieval and embryo transfer. All told, one cycle of IVF takes around two months. Continue reading for an overview of each step of the IVF process.
Preparing Your Cycle Before Treatment
There are a few steps to take before beginning IVF treatment that are important to know about. Your doctor will want to know how to predict your cycle so he or she knows when ovulation is expected to occur. If you have regular cycles, you may be asked to chart your temperature or to detect when ovulation begins. Some doctors may ask you to start birth control pills during the cycle before treatment. This may sound counterintuitive for someone trying to become pregnant, but it can improve your odds of success and decrease your risk of ovarian hyperstimulation syndrome.
The key to this stage prior to beginning treatment is that your doctor needs to establish control over when you ovulate. After you ovulate, your doctor will start you on medications to stimulate ovulation.
When The Treatment Starts
Your treatment cycle officially starts on the first day of your period after beginning medications. At this point, it’s time for your baseline bloodwork and baseline ultrasound. On day two of your period, your doctor will conduct a blood test and a transvaginal ultrasound to check the size of your ovaries and your estrogen levels and to look for any ovarian cysts that might be present. If everything looks okay, your doctor will clear you to proceed!
Ovarian Stimulation and Monitoring
Once the doctor has given you the green light to proceed, you will begin taking medications to increase your egg production. Normally, your body releases one egg each cycle. With IVF, your chances of success increase when you have multiple eggs to choose from. Not every egg will be viable, which is why you’ll need to take medications to signal your body to produce more.
During this stage, your doctor will monitor how your body responds to the medication and will make adjustments as needed. He or she will need to monitor how your ovarian follicles are developing so your medication dosages can be increased or decreased accordingly. You will likely be making daily trips to your IVF clinic to complete this monitoring for bloodwork and ultrasounds.
Oocyte Maturation
Now that your body is producing several eggs, or oocytes, you’ll need to make sure they reach a proper level of maturation. Your doctor needs to be sure that the eggs are fully ready to be retrieved, so you’ll be given what’s called a trigger shot to self-inject at a precise time.
The trigger shot contains human chorionic gonadotropin (hCG) which gives your eggs a boost to reach full maturity. The timing of this shot is super important! If you are off by a little as an hour, your eggs may be too immature or too over-developed to fertilize successfully.
Egg Retrieval
Roughly 36 hours after your trigger shot, your doctor will perform the egg retrieval procedure at your clinic. The actual egg retrieval process takes only 20 minutes (though you should plan to be at the office for around three hours that day), and takes place in their ambulatory surgery center.
You’ll be given mild IV sedation (not general anesthesia), so you won’t feel anything during the procedure. You may feel crampy the day after, and most women choose to take 1–2 narcotic painkillers the day of the egg retrieval, possibly one more the next day, and then ibuprofen if anything, the day after. It’s best to rest and relax at home for a day or two, but most women are back to their daily routine after a few short days. You’ll need to have someone who can drive you home following the procedure, so plan to bring a friend or family member.
Once you are comfortable, the doctor will use a transvaginal ultrasound probe to guide a needle to your ovaries. Then, the follicle is aspirated to gently remove the egg from the follicle. This is repeated for each follicle, with the doctor carefully removing each egg to be transferred to the embryology lab for the next step. On average, about 8 to 15 eggs are retrieved during this procedure.
Following the procedure, clinic staff will monitor you for an hour or so to make sure no complications arise. It’s recommended that you spend a day or two resting at home, so use this time to catch up on Netflix!
The egg retrieval process is the same whether you are completing the procedure as an intended mother or as an egg donor. Interested in becoming an egg donor? Learn more about the entire egg donor experience at FamilyInceptions.com.
Fertilization
After the egg retrieval, your clinic’s embryologist will evaluate the quality of the eggs. Once they’ve determined which eggs are properly mature and likely to be viable, the fertilization process can begin. This has to happen within 12 to 24 hours after retrieval.
Collecting Sperm
There are two possible ways to obtain the sperm that will be used to fertilize the eggs. If you have a male partner, he will be asked to give a sperm sample to be used. Many clinics prefer for the sample to be given the day of fertilization, but it can also be provided and frozen in advance.
The other option is to use donor sperm that you arrange for with the help of a sperm bank or a known donor.
Uniting The Sperm and Egg
The embryologist will perform a special washing process on the sperm in order to extract just the single sex cells. After choosing the most viable-looking sperm, the embryologist will put about 10,000 sperm cells into a petri dish with a single oocyte (egg). These get placed in a special incubator and then checked for signs of fertilization after 12-24 hours.
It’s Time to Transfer The Embryo
Three to five days after the egg retrieval, it’s time to look for healthy embryos! Your embryologist will visually inspect each petri dish to see which cells have combined to form the earliest stage of an embryo: a blastocyst. Sometimes, genetic screening is performed to check for any possible defects or hereditary conditions.
You’ll prepare for the embryo transfer procedure in much the same way as you did for the embryo. You’ll need to have someone to drive you home, and you will be given a light sedative. Your doctor will pass a catheter (a thin tube) through your cervix in order to insert the embryos and a small amount of fluid into your uterus.
After the transfer, you will need to lie down for a few hours before heading home. Clinic staff will check in on you regularly to make sure you’re feeling okay and there are no signs of complications. Following the procedure, you may experience cramping, spotting, or mild discomfort.
After Treatment and Progesterone Support
Now begins the infamous two-week wait! Your doctor will likely prescribe progesterone injections or support to help your body maintain the best hormone levels to promote pregnancy. This period of time can be stressful as you wait to find out if the embryo has implanted. Plan something to take your mind off of the wait. It helps a lot of people to keep busy and a little bit distracted from thinking about the possibility for success.
As you wait, the embryo will begin to attach to the lining of your uterus. Some women can experience light spotting, known as implantation bleeding, tender breasts, or light cramping. The only way to detect pregnancy is with a blood test after about two weeks, so try not to analyze every possible symptom. It’s hard, we know!
Pregnancy Tests and Follow-ups
9 to 12 days after the transfer, you’ll have a blood test to detect pregnancy. If the test is positive, your doctor will continue to monitor your hormone levels and will follow up with additional blood work and ultrasounds to make sure the pregnancy is progressing as it should.
When Treatment Fails
Of course, there is a possibility that your embryo transfer and IVF treatment won’t be successful. If, after 12 to 14 days, you are still receiving negative tests, you’ll need to stop the progesterone treatment and wait for your period to begin. This can be a heartbreaking outcome, but please know that you can likely try again, and in fact, your chances for success can increase with each additional cycle.
Your doctor may recommend additional testing to help find new solutions or treatments that may increase your chances. Some possibilities include using different medications, having genetic screening done, immunotherapy, or other alternatives.
Possible Pregnancy Risk from IVF Treatment
There are some pregnancy risks to be aware of. The IVF process makes it more likely that you will become pregnant with multiples. The chance of becoming pregnant with multiples increases greatly if you choose to transfer more than one embryo. You will need to discuss this possible outcome with your doctor before you begin treatment. If the plan is to transfer multiple embryos, you will need to think about possible risks associated with carrying twins, triplets, or more.
Women who carry multiples are at greater risk of premature labor and delivery, hemorrhage, gestational hypertension, gestational diabetes, and C-section delivery. Because of the associated risks, many clinics have policies in place to only transfer one embryo, greatly reducing the chance of multiples. Should you experience a higher-order pregnancy of 4 or more, you will likely be encouraged to consider selective reduction. Higher-order pregnancies are very risky for the health of the mother and the fetuses.
Other risks remain similar to pregnancies that were achieved without IVF. The rate of miscarriage remains the same and varies mostly based on the age of the mother. Ectopic pregnancy occurs in 2-4% of all IVF conceptions, though this is not significantly higher than the rate with natural conception.
Can IVF Treat Infertility?
IVF is a common method for treating infertility, but it’s not usually the first treatment to be tried. People experiencing infertility may try fertility medications to assist with becoming pregnant. Other infertility treatments include surgery or artificial insemination. The course of treatment depends in large part on the cause of your infertility.
IVF can help treat infertility caused by the following:
- Low sperm counts
- Low sperm mobility
- Abnormal sperm
- Endometriosis
- Problems with the uterus or fallopian tubes
- Ovulation disorders such as PCOS
- Antibody problems that harm sperm or eggs
- Inability of sperm to penetrate or survive in the cervical mucus
- Poor egg quality
- Genetic disease of one or both intended parents
- An unexplained fertility problem
Infertility is generally diagnosed if you have been having unprotected sex for 12 months or more without becoming pregnant.
Of course, IVF also makes it possible for gay men and single men to have a biological child by working in conjunction with a gestational carrier. Learn more about becoming a parent via gestational surrogacy at FamilyInceptions.com.
IVF vs IVM
In Vitro Maturation is a process in which eggs are collected and then matured in the lab, outside of a woman’s body. You’ll recall from the process described above that during IVF, a patient is given a trigger shot of hormones to cause the eggs to mature right before retrieval. IVM eliminates this step, which makes it a good choice for women who have PCOS or who are at a higher risk for ovarian hyperstimulation syndrome.
IVM can also be used when immature eggs are retrieved during the IVF process. Traditionally, an embryologist would have to discard any immature eggs, but with IVF, they can employ the IVM process to try and speed up maturation outside of the body.
Because IVM requires fewer medications, it is less expensive than IVF. It is also a shorter process, so it’s often a good option for women who want to have their eggs retrieved and then frozen for future use without going through the entire IVF process. IVM allows women who suffer from cancer to preserve their eggs for future use before undergoing chemotherapy.
And The Ultimate Question: How Much Does It Cost?
IVF treatment can be very expensive. A single cycle costs $15,000 or more. One study found that the average amount spent out-of-pocket on IVF is close to $19,000. There are a few states that require insurance companies to provide coverage for IVF, but for the most part, patients will need to pay for the treatment out-of-pocket. Check with your insurance company, though, because sometimes a portion of the treatment will be covered. Lab tests, medications, or ultrasounds may be covered, for example.
There are some ways to save on the cost of IVF treatment and to make it more affordable. There are fertility scholarships and grants you could apply for, or some people raise funds from family and friends. Some clinics also offer shared risk programs or IVF refund programs that could help you minimize costs.
Should I Pursue IVF Treatment?
The choice of whether or not to pursue IVF treatment is emotional and highly personal. If you are struggling with infertility, we encourage you to reach out to your doctor to discuss your options. The journey to parenthood isn’t always easy, but it is worth it. If we can help you at all along the way, please don’t hesitate to reach out.